What Is a Thromboembolism, and How Does It Affect Gynecologic Surgery?
Venous thromboembolic events (VTE) refers to pulmonary embolism (PE) and deep vein thrombosis (DVT). Despite advancements in prevention, diagnosis, and therapy, VTE is a primary source of cost, disability, and death in postoperative and hospitalized gynecologic patients. In addition, other chronic illnesses may develop due to acute disorders like post-thrombotic syndrome, venous insufficiency, and pulmonary hypertension.
Some current methods to prevent venous thromboembolism include-
-
Mechanical prophylaxis.
-
Preoperative pharmacologic prophylaxis.
-
Postoperative pharmacologic prophylaxis.
-
Extended duration pharmacologic prophylaxis (patient can continue these medications at home after hospital release).
Who Is at Risk of Developing Thromboembolism During Gynecologic Surgery?
-
For patients with gynecologic malignancies, venous thromboembolism is a major source of morbidity and mortality. Gynecologic oncology patients are a particularly high-risk category due to the recognized increased risk of venous thromboembolism in patients with malignancies and those following pelvic surgery.
-
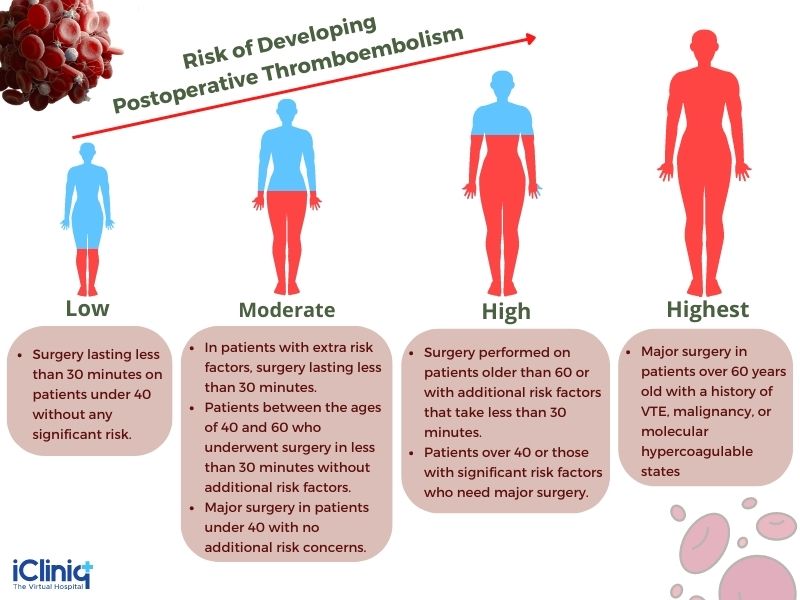
Patients undergoing gynecologic surgery have been preoperatively categorized into four risk categories: low, medium, high, and greatest risk. The best thromboprophylaxis treatment for a given patient is chosen using this classification. The risk of venous thromboembolism (VTE) is established based on the kind and length of the surgery, the patient's age, and the presence of additional risk factors.
-
For patients having surgery, the American College of Chest Physicians (ACCP) advises using risk assessment tools to determine their risk of developing postoperative venous thromboembolism. It is determined as-
-
The Caprini score and the Rogers score are two distinct risk assessment measures that the ACCP advises should be used to place patients into these risk groups. Based on patient and procedure risk factors linked to venous thromboembolism, both risk assessment methods offer a score. These scores give each risk factor a relative weight in the form of points, formalizing the correlations between multiple risk factors for venous thromboembolism that have been established in substantial research.
1. The Caprini Score- Each patient is classified as having a low, moderate, high, or very high risk of developing venous thromboembolism based on their score, which is given points for several venous thromboembolism risk factors. The score has the advantage of being simple to use, and several surgical specialties have utilized it in practice.

2. The Rogers Score-Various patient and procedure risk variables are given points. Based on their final results, patients are divided into risk groups. Patients with scores of less than seven are at low risk, between seven and ten are at moderate risk, and greater than ten are considered to be at high risk. The Caprini score is more commonly utilized than the Rogers score.

-
Identifying patients who are more likely to experience venous thromboembolism and administering prophylaxis to lower that risk in those populations makes risk assessment technologies potentially helpful and advised.
-
Additionally, people with a decreased chance of having venous thromboembolism are identified using risk assessment techniques. By identifying people with lesser risk, practitioners can avoid preventative procedures that are expensive and have dangers for those who are less likely to benefit, including increased bleeding.
-
Clinicians can maximize the advantages of prophylaxis and reduce the risks by using a targeted prophylaxis regimen that is adjusted to patient- and procedure-specific risk factors.
What Are the Various Prophylaxis Strategies Used to Prevent Thromboembolism in Gynecological Surgery?
The prevention of venous thromboembolism is mostly not universal. However, the risk of postoperative venous thromboembolism can be reduced by using various therapies and tactics. These include extended duration pharmacologic prophylaxis that the patient continues at home after being discharged from the hospital, preoperative pharmacologic prophylaxis, postoperative pharmacologic prophylaxis, and mechanical prophylaxis.
-
Mechanical Prophylaxis- The main goal of mechanical prophylaxis techniques is to reduce the venous stasis that raises the risk of postoperative venous thromboembolism. Mechanical prophylaxis techniques that reduce venous stasis fall into two categories:
-
Passive Methods- The use of graded compression stockings is one passive strategy. The benefits of graduated compression stockings include their simplicity and low price. In most cases, postoperative DVT appears 24 hours after surgery. Graduated compression stockings prevent blood clotting in the calf veins.
Gradual compression stockings have several disadvantages, such as incorrect fitting, where the stockings could function as a tourniquet and cause venous stasis. As a result, knee-length stockings are advised. Additionally, graduated compression stockings have been linked to a higher risk of skin issues like necrosis, ulcers, and blisters.
-
Active Methods- Devices like intermittent pneumatic compression devices (IPC), which actively compress and release to provide pulsatile flow out of the lower extremities, are examples of active approaches. Until a postoperative patient is completely mobile and prepared for discharge from the hospital, IPC should be worn continually on the calf muscles.
-
Pharmacologic Prophylaxis Strategies- Pharmacological techniques work at various points throughout the coagulation cascade to inhibit clot formation.
The following pharmacologic prophylaxis agents are used,
-
Low-dose unfractionated heparin (LDUH)
-
Low molecular weight heparin (LMWH).
-
Direct thrombin and factor Xa inhibitors.
Timing of Pharmacologic Prophylaxis: There are two problems regarding the ideal time to start perioperative thromboprophylaxis. The first is whether preoperative pharmaceutical prophylaxis in addition to postoperative prophylaxis is required. The second is whether there is a recommended window of time after surgery before administering the initial dose of postoperative pharmacologic prophylaxis. Waiting too long could allow thrombosis to form, and starting therapy too soon could raise the risk of bleeding and the associated consequences.
-
Dual Prophylaxis- Dual prophylaxis is the simultaneous application of mechanical and pharmacologic prophylaxis. Dual prophylaxis is vital to understand since it can refer to either a technique in which mechanical prophylaxis is paired with medication administered only after surgery or a strategy in which mechanical prophylaxis is combined with both preoperative and postoperative medication.
-
Extended Duration Prophylaxis- It is a method to decrease fatal thromboembolism episodes. Postoperative extended duration pharmacologic prophylaxis is administered at home after the patient is discharged from the hospital.
Conclusion:
For patients with gynecologic surgery, venous thromboembolism is a major cause of morbidity and mortality. A dual prophylaxis strategy is preferred for most gynecologic patients having laparotomies. Additionally, pharmacologic prophylaxis before surgery is probably advantageous for these individuals. Given the lower risk of venous thromboembolism in patients with gynecologic cancer undergoing minimally invasive surgery, less prophylaxis is perhaps necessary. It has been demonstrated that a wide range of preventative therapies against venous thromboembolism (VTE) can lessen the development of deep vein thrombosis (DVT). However, the main goal of VTE prevention is to shield patients undergoing gynecologic surgery against deadly PE.











