Introduction:
Neurosurgical anesthetist requires deep knowledge and understanding of the normal anatomy and physiology of the central nervous system and the alterations that occur during a space-occupying lesion, trauma, or infection. Patients with mobility problems and other chronic illnesses are being treated more often with functional stereotactic neurosurgery. The anesthesia for neurosurgery, principally intracranial surgeries, needs to be administered under circumstances that keep the blood supply intact to the brain.
The exploration of new combination techniques with short-acting anesthetic agents, regional anesthesia, and better infusion and monitoring techniques is a way to improve the management modalities of neurosurgical anesthesia. Furthermore, for a smooth induction and emergence of anesthesia, it is important to pay close attention to maintaining a healthy cerebral perfusion pressure (CPP), avoiding intracranial hypertension, and setting up the best possible surgical conditions to stop the progression of the initial neurological insult. Neuro anesthesia is challenging because clear unexpected demands have to be taken care of during surgeries. The most characteristic feature of neuro anesthesia is that importance is given to both sending them to sleep as well as to waking the patient after the procedure.
What Are the Objectives of Neuro Anesthesia?
The four main objectives of neuro anesthesia are:
-
The maintenance of adequate cerebral perfusion pressure (CPP) and balanced intracranial pressure (ICP).
-
Establishing better surgical conditions.
-
Make sure the patient is sufficiently anesthetized without any straining or coughing.
-
Establishing a rapid return to consciousness after surgery for neurological assessment postoperatively.
What Are the Physiological Principles of Neurosurgical Anesthesia?
Sufficient blood supply maintenance to the brain is the foundation for neurosurgical anesthetists. Under normal conditions, 15 % of cardiac output, or 700ml/min, is made up of cerebral blood flow (CBF), which is equal to 50ml/100g of brain tissue per minute. The brain weighs about two percent of the total body weight (~1350 gm). In order to maintain cellular homeostatic functions, 40 % is used by the brain tissues, and 60 % of the total energy is needed for the maintenance of the electrophysiological function of the brain, like depolarization - repolarization, uptake, and transport of neurotransmitters.
How Does Cerebral Blood Flow Regulation Take Place?
The cranial vault houses the brain and has a fixed volume. Thus, the pressure inside the cranial vault has an impact on cerebral blood flow (CBF); below this, the function of the brain declines. CBF counting both gray matter and white matter account for about 675ml/min in case CBF drops to 20ml/100gm of brain tissue per minute, leading to ischemia of the brain, and when CBF falls below 10ml/100gm of brain tissue per minute, leads to irreversible damage to the brain. Cerebral perfusion pressure is the effective pressure that causes blood flow to the brain and is a useful measure of this pressure. Hence cerebral perfusion pressure (CPP) is the difference between the mean arterial pressure (MAP) and the sum of the intracranial pressure and the central venous pressure (CVP).
CPP = MAP - (ICP + CVP)
In a healthy individual, the ICP remains at 5 to 12 mmHg, the venous pressure at the base of the skull is zero, and CPP varies depending on the person's MAP.
Autoregulation - CBF depends on chemical, myogenic, neurogenic, and a few extrinsic mechanisms.
Which Is an Ideal Anesthetic Agent?
The anesthetic agent should have a remarkable impact on the outcome of the surgery. The ideal anesthetic agent should possess the following features: rapid onset and rapid emergence for neurological assessment, hemodynamic stability, and ICP reduction.
Interdependence exists between cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2). Flow-metabolism coupling is a phenomenon whereby an increase or reduction in the brain’s metabolic oxygen demand would increase or decrease the CBF accordingly. As the skull is a closed cavity, any rise in CBF will also raise ICP and have an impact on CPP.
What Are the Effects of Anesthetic Agents on Cerebral Blood Flow?
Anesthetic agents cause a reduction in neuronal activity and thereby cause a reduction in the cerebral metabolic rate of oxygen (CMR02).
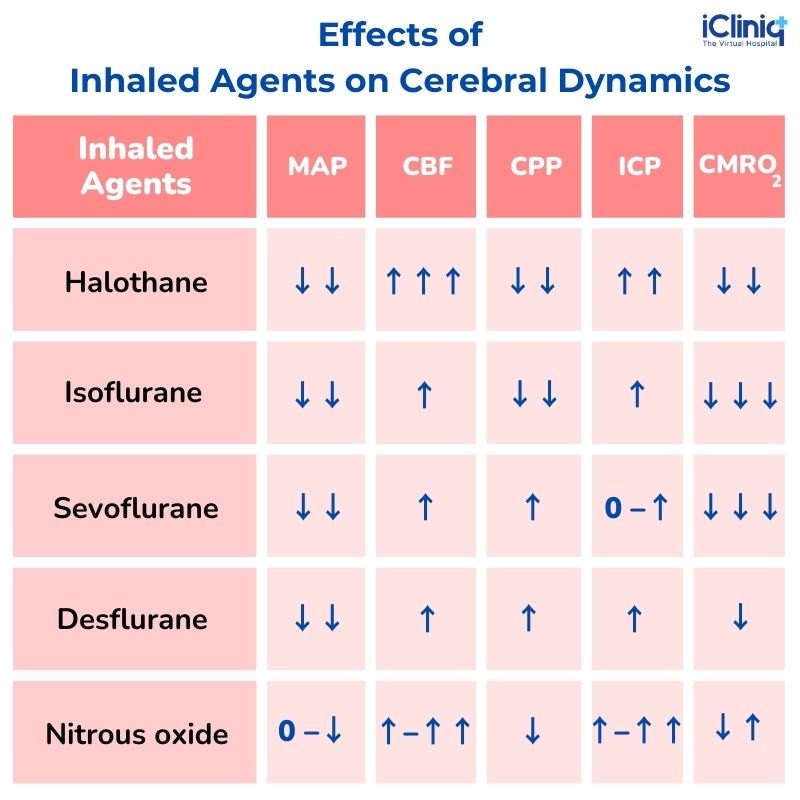
What Are the Effects of Inhaled Agents on Cerebral Dynamics?
What Are the Effects of Intravenous Agents on Cerebral Dynamics?

CBF - cerebral blood flow; CMRO2 - a cerebral metabolic rate of oxygen; CPP-cerebral perfusion pressure; ICP-intracranial pressure; MAP-mean arterial pressure.
What Is the Anesthetic Evaluation for Neurosurgery?
1. Preoperative Evaluation of a Patient Undergoing Neurosurgery:
-
Along with the routine evaluation, the patient should be assessed for signs of elevated ICP, such as (nausea or vomiting, hypertension, bradycardia, papilledema, headache, altered consciousness, and breathing.)
-
Cardiac complications should be evaluated before surgery.
-
Patients undergoing spine surgery have weakness or paralysis, which is not indicated for Succinylcholine.
-
Neurosurgical patients taking antiepileptic drugs such as Phenytoin should be evaluated.
-
Patients taking antihypertensive drugs, hyperglycemic drugs, and anticoagulants are to be considered.
2. Induction and Airway Management of Patients Undergoing Neurosurgery:
-
Induction is a critical step for patients with elevated ICP and altered cerebral pressure.
-
During induction and intubation, low levels of oxygen in the brain tissue, increased carbon dioxide in the bloodstream, and vasodilating agents should also be avoided.
-
Thiopentone, Propofol, and Etomidate are the most widely used anesthetic agents useful in neurosurgical procedures.
-
Hypotension, hypertension, and apnea are the dangerous effects caused due during the administration of anesthesia.
3. Positioning of the Patient:
-
The neurosurgical anesthetist has limited access to the patient’s head. The endotracheal tube should be secured carefully before draping. In order to prevent tangling, the breathing circuit, monitor cables, and intravenous and intra-arterial lines with appropriate extension lines should be arranged.
-
Supine - for frontal, temporal, or parietal access; semilateral- for retromastoid procedures; lateral-for posterior parietal and occipital access; prone - for spinal, occipital, cranial suture, and posterior fossa procedures; sitting - for some posterior fossa and cervical spine surgery; head frame position.
4. Maintenance of Anesthesia:
-
The following factors should be considered for the maintenance of anesthesia - stable arterial BP, normal ICP, normal CPP, reduction of cerebral swelling, and maintenance of adequate blood supply to the brain.
-
The airways, venous access, and monitoring lines should be secured properly during the administration of neurosurgical anesthesia.
What Are the Complications of Neurosurgical Anesthesia?
Hypertension, hypotension, arrhythmia, obstruction of the airway, pain, nausea, vomiting, postoperative shivering, and seizures.
Conclusion:
Neurosurgical anesthesia is developing rapidly, and it provides neuro anesthetists with new challenges in the surgical field. A thorough understanding of anatomical, metabolic, and neurological abnormalities is required for the complicated and challenging task of managing neurosurgical patients.












